As we have see in part 1 patellofemoral pain (PFP) is multifactorial, making it challenging to treat. Despite the high prevalence among the sporting population, there are few published guidelines determining the most appropriate evidenced based treatment. A recent paper by Barton et. al (2015) recommends individually tailored programmes with the emphasis on active exercise rehabilitation and education.
Treatment Options:
Load Management:
Modifying the aggravating exercise or activity is one of the first recommendations to help reduce pain. Depending on the severity of your symptoms you might only need to reduce the frequency or intensity of the activity. Alternatively, you may need to stop the activity for a short period to allow the knee to settle. This does not mean complete rest, taking part in active rehabilitation is key to the succsessful long term outcome of this condition.
Exercises:
To reduce pain in the short, medium and long term and improve function, exercise therapy is the most important recommendation. A combined approach targeting the strength of the hip and knee muscles has shown the greatest evidence for improving PFP.
Knee (Quadriceps) Exercises:
If you are in severe pain you may need to start with very low load activation exercises such as sitting and tightening the quadriceps muscles or extending the knee from a seated position. As pain tolerance improves weight bearing exercises such as squats, step ups and lunges are great at improving the strength of the quadriceps. Eventually you will want to include exercises which replicate your day to day and sporting activity.


Ball Squatting is a great early weight bearing exercise. This encourages both the gluteals and the quadriceps to accept load.
As a progression the Step rock and Step up starts to introduce unilateral strength and control to the hip and knee muscles.
Hip (gluteal strengthening) exercises:
Strengthening the hip muscles is a vital component to the management of patellofemoral pain (Crossley et al 2016). Non weight bearing exercises targeting the whole gluteal complex are considered in the early phase of training. However, weight bearing hip strengthening exercises should be performed as soon as they are tolerated. The emphasis should be on maintaining good alignment of the lower limb avoiding the knee and hip rolling inwards. For guidance using evidence based gluteal exercises, Tom Goom aka running physio has produced this excellent circuit.
Progression of Exercises:
Progression should only happen in the absence of significant pain and the ability to maintain control and be guided by your physiotherapist. Closing the eyes whilst for example whilst doing a lunge will challenge the balance systems. Adding weight increases the strength, whilst adding pulses in a squat will challenge the adaptability and elasticity of the muscles. The demands of the sport should dictate the final progressions of rehabilitation. You may need to be guided by your physio or therapist as to how to progress your rehabilitation safely.
Run Retraining:
The aim of running retraining is to reduce the forces being placed through the patellofemoral joint and to reduce excess inward rotation of the of the thigh. Increasing step rate by 5%-10% and transitioning from a rear foot to a more midfoot strike pattern has been show to reduce PFP. Using visual and verbal cues can also be helpful such as “open the knees” or “land softly and quietly”. Using technology tools such as the Run Cadance app are designed to help improve your cadence by setting the correct beat. If you would like more detail on running retraining training please visit this article I wrote previously .
Stretching:
There is less evidence indicating the effectiveness for stretching for patellofemoral pain, however, it is something you should consider, especially if you tight in and around the knee, hip and calf muscles. Restriction in these muscles can affect the position and pull of the patella and increase compression of the patella against the femur. Tight calfs will cause increased knee bend and can lead to increased foot pronation.
Pain monitoring system:
In addition, using a visual pain scale to monitor pain levels when exercising can help avoid pain-induced muscle inhibition.
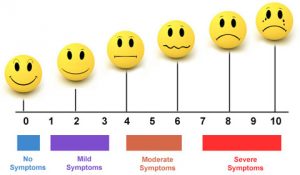
Keeping pain at or below 3/10 during and after exercise will keep you in the safe zone, and, therefore, less likley to cause further harm to your knee. Pain levels up to 5/10 momentarily during exercise or immediately following exercise are acceptable, but not extending into the following morning.
Passive Treatments:
Passive treatments include taping, braces and orthotics and may reduce pain in the short term. Taping is used to off load or change the direction of pull of the patella. Ideally your physiotherapist should show you a simple taping technique which you can then replicate at home. This video explains more.
Key Take Home Messages:
- If you have patellofemoral pain see help as early as possible to help improve your chances of recovery.
- Often, the first step to successful recovery is to modify your physical activity in the short term.
- It is absolutely key that you make every effort to participate in your rehabilitation.
- Hip and knee exercises are vital to the rehabilitation process.
- Movement retraining and run retraining can also be beneficial and reducing pain related activity.
- It is very important to build up your physical activity gradually.
